
CIRCUMCISION
What is Circumcision?
Male circumcision is the removal of the foreskin from the human penis. Boys are born with a hood of skin, called the foreskin, covering the head (also called the glans) of the penis. In the most common procedure, the foreskin is surgically removed; exposing the end of the penis and the foreskin is separated from the glans.
General description
The aim of the procedure is surgical removal of the foreskin. The operation is performed as a day-case under general anaesthesia. The operation usually takes about 30 minutes.
Preparations
Your child will need to fast for solids and liquids generally for about 6 hours before the start of the procedure. In breast-fed babies or infants this time may be reduced after consultation with the anaesthetist. Please ring the Day Surgery Unit one working day before surgery to confirm these times. It is often helpful to bring your child’s favourite toy with you on the day.
Anaesthesia
You and your child will meet the anaesthetist prior to the procedure. After talking to you and briefly examining your child, they will take you through to the operating theatre. One parent is welcome to accompany your child until they are asleep. The anaesthetist puts your child to sleep via a face mask (with children 5 years and over there is the option of either a face mask or a needle with numbing cream). You will then be shown the waiting room where there is tea, coffee or water available to drink.
Once your child is asleep, the anaesthetist will insert a ‘drip’ to allow fluids to be given directly into a vein. Usually this is located in the hand or arm, but occasionally may need to be sited in the leg or scalp. The anaesthetist will then inject some local anaesthetic to numb the penis. Usually this is injected around the base of the penis, but occasionally it may be given near the base of the spine near the ‘tail’ bone, termed a ‘Caudal’. Please inform the anaesthetist if you wish to discuss the relative risks and benefits of these two options.
Procedure
The penis is cleaned with an antiseptic solution. The foreskin is removed and any bleeding stopped with an electrical cautery instrument. The wound is then closed using a pale yellow stitch material that will dissolve slowly over the next 2 to 6 weeks. No dressing is used, but an antibiotic ointment is applied to the wound to help prevent infection.
Initial recovery
Once the operation has finished, your child will be taken to the recovery area. When they are awake, you will be called into the recovery ward. Often children appear distressed and a little confused initially – there may be several reasons for this including residual effects of the anaesthetic, hunger, and some discomfort. Generally they will settle quite quickly, especially if offered a drink or feed. The recovery and ward staff are also able to give pain relief medication once your child is awake, and this is sometimes required. The nursing staff will check the wound and make sure you are happy before you go home. Usually this will be about 2 hours after the surgery.
Post-operative course
There may be a small amount of blood that oozes from the wound, enough to lightly stain a nappy or pair of under pants. Any further bleeding should be discussed with your local doctor or myself. Paracetamol (‘Panadol’) should be given on the afternoon and evening of surgery, and in the morning of the following day. After that time, assess your child’s pain to see if further doses are required. Children over 12 months of age may require stronger analgesia such as ‘Painstop Day-time’ (or ‘Painstop Night-time’ if over one year of age) for the first day or so. For either Panadol or Painstop Day-time, follow the manufacturer’s dose instruction but never give more than 4 doses in a 24-hour period and never both at the same time.
Your child should not be bathed on the first night, but nappies can be changed as required and a ‘wetwipe’ or similar cloth used. Normal bathing is safe from the next day onwards. It is important to apply the tube of topical antibiotic cream (‘Chlorsig’) supplied to the wound 2 to 3 times a day for 1 week. In addition, to help prevent the tip of the penis from sticking to underpants or nappies, a thin layer of ‘Vaseline’ or petroleum jelly is helpful. When your child passes urine, the stream may be difficult to control at first. It may also be deflected to one side or another for the first week or so. This is because of the normal swelling following surgery and is no cause for concern.
Often the tip of the penis, called the glans, will appear red, swollen and ulcerated in the first few weeks after surgery. A white layer of fibrin may

also appear to cover the head of the penis. This is normal and does not represent infection. The covering of the glans needs to change from a protected moist covering, like the inside of the mouth, to dry skin like the rest of the body. The swelling improves considerably after the first week but does not resolve completely for up to 8 weeks after surgery.
Your child will begin eating once awake after surgery. Start with clear liquids (apple juice, iceblocks) and add solid food slowly and in small amounts. Your child may vomit from the anaesthesia on the day of surgery. This should stop by the morning after surgery.
Return to activity
Your child may return to day care or school when comfortable, usually within 3-5 days. He should not participate in sports or swimming for 3 weeks after the surgery and should not ride straddle toys (bikes, walkers) for 2 full weeks after surgery. You should continue to use your car seat.
Call our office or emergency department on given numbers if:
- You see any signs of infection
- Your child’s pain gets worse or is not relieved by painkillers
- There is bleeding (small ooze of blood in the first day or two is normal)
- Your child has a high temperature
- Ongoing vomiting or failure to tolerate fluids on the day following surgery
- You have any questions or concerns
Follow up 4-6 weeks after surgery.
Follow-up
Normally I see you and your child about 4-6 weeks following surgery. This is both to ensure that the wound has healed and that you and your son are satisfied with the results of the operation. For patients from rural areas, this review may be deferred to your own general practitioner if you prefer. Please ring soon after the operation to book the post operative appointment to arrange a convenient time.
Problems & further surgery
The most common problem following a circumcision is bleeding, occurring in 5% of boys. Some oozing from the wound is normal after the surgery for the first 24- 48 hours. This should not be a steady trickle, however, and if this occurs please contact my rooms or present to the Emergency Department of your local hospital. Generally bleeding can be stopped with pressure or a special dressing. Rarely your son will need to return to theatre for a second operation to stop the bleeding. Parents are often concerned about redness and crusting of the wound and the glans or ‘head’ of the penis in the first week or so. The wound may also appear white and quite moist. This is part of the normal healing process and does not represent infection. Remember the skin of the glans of the penis needs to adapt from being soft, moist skin to tough, dry skin. This process normally takes a few weeks. Infection, if it occurs, usually happens between four and seven days following surgery. It is suggested by a thick, yellow discharge from the wound; pain, fever and increasing redness around the wound. Rarely, parents may be dissatisfied with the cosmetic outcome of the procedure. Generally the scarring will improve with time. A revision circumcision would normally only be considered if the results remain unsatisfactory after the scar maturation process is complete 12 months following surgery.
ORCHIDOPEXY
What is an undescended testis?
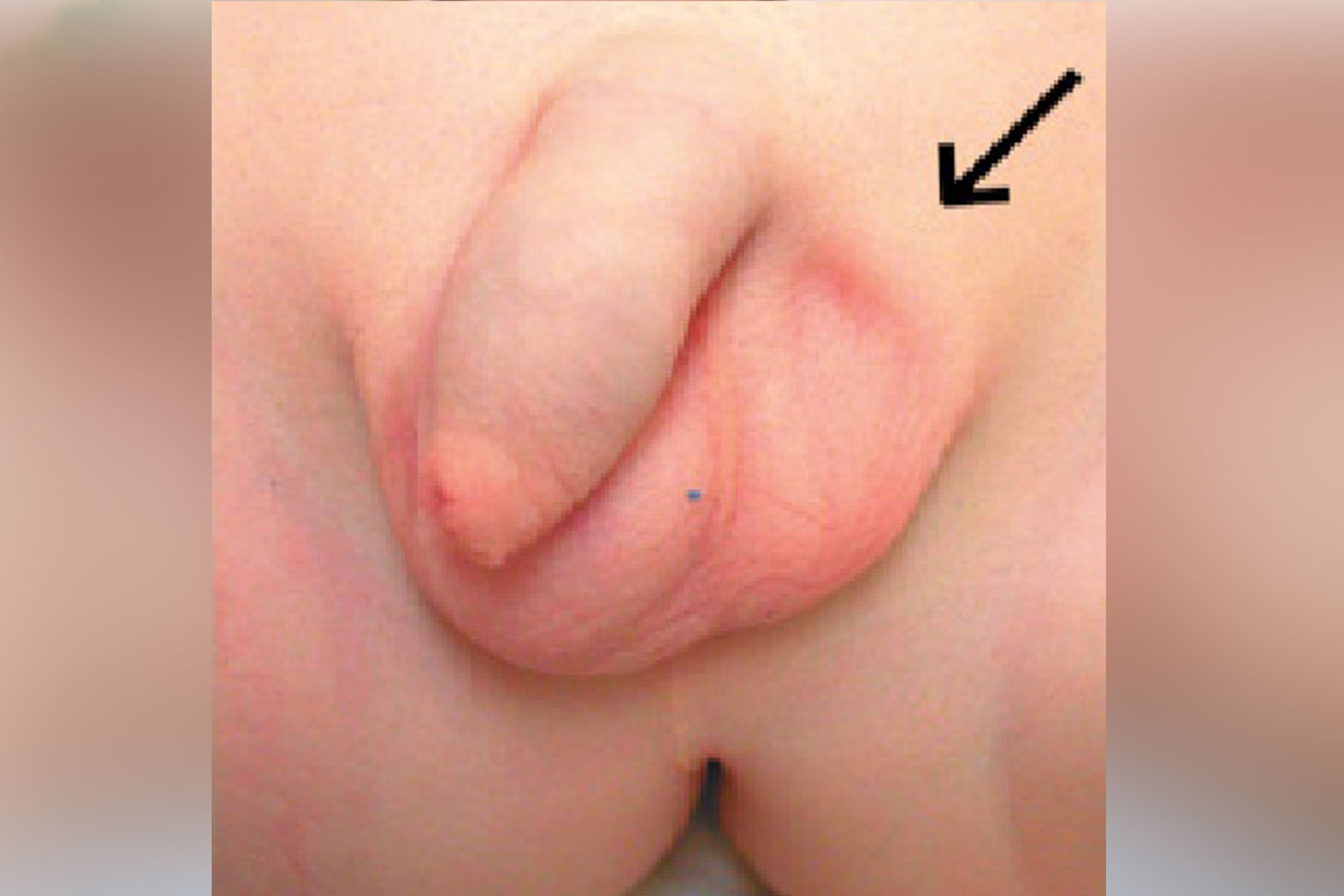
An undescended testis is when the testis is not fully down in the boy’s scrotum. The testis first develops near the kidney when the baby boy is inside the mother’s womb. For the testis to drop down into the scrotum there needs to be a passage through the groin area. Sometimes the testis remains inside the tummy cavity, but much more commonly it becomes stuck in or close to the groin passage. An undescended testis is not uncommon at birth, especially in premature boys. The testis may ‘drop’ of its own accord in the first 6 months of life, but is very unlikely to do so after this time. The testis needs to be located in the scrotum in
order for it to be kept cooler than the rest of the body and to produce normal sperm when the boy is older. Ideally this operation should be performed before the boy is 12 months of age.
General description
The aim of the procedure is to fix the testis in the scrotum. The operation is performed as a day-case under general anaesthesia. Generally the operation takes about 45 minutes.
Preparations
Your child will need to fast for solids and liquids generally for about 6 hours before the start of the procedure. In breast-fed infants this time may be reduced after consultation with the anaesthetist. Please ring the Day Surgery Unit the working day before surgery to confirm these times. It is often helpful to bring your child’s favourite toy with you on the day.
Anaesthesia
You and your child will meet the anaesthetist on the morning of the procedure. After talking to you and briefly examining your child, they will take you through to the operating theatre. One parent is welcome to accompany your child until they are asleep. The anaesthetist puts your child to sleep via a face mask (with children 5 years and over there is the option of a face mask or a needle with numbing cream). You will then be shown the waiting room where there is tea, coffee or chilled water available to drink. Once your child is asleep, the anaesthetist will insert a ‘drip’ to allow fluids to be given directly into a vein. Usually this is located in the hand or arm, but occasionally may need to be sited in the leg or scalp.
Procedure
The groin area and scrotum is cleaned with an antiseptic solution. A local anaesthetic block is injected into the area so that the site of the operation is numb after the operation. This block usually lasts for about 4 to 6 hours. A cut is made in the groin on the side of the undescended testis, with a second smaller cut at the bottom of the scrotum on the same side. Once the testis has been found, it needs to be carefully released so that it can be brought into the scrotum. This will often involve removing a small hernia near the testis. The hernia must be peeled off two important tubes: the blood vessel to the testis and the sperm tube. This usually allows the testis to be placed in the scrotum. The wounds can then be closed with dissolving stitches which are buried under the skin in the groin but which will be visible in the scrotum. A clear water resistant dressing is then placed over each wound.
If the testis is very high in the groin or inside the abdominal cavity, a laparoscopic orchidopexy may be performed. This involves inserting a small telescope through the umbilicus, with typically two further incisions about 5mm in size in the lower in the abdomen for special instruments to enable the testis to be mobilised into the scrotum. If the blood vessel to the testis is very short, occasionally two operations approximately 3 months apart may be required for the best chances of success.
Initial recovery
After the operation has finished, your child will be taken to the recovery area. Once awake, you will be called into the recovery ward. Often children appear mildly distressed and a little confused initially. There may be several reasons for this, including residual effects of the anaesthetic, hunger and some discomfort. Generally they will settle quite quickly, especially if offered a drink or feed. The recovery ward staff are also able to give pain relief medication once your child is awake and sometimes this is required. The ward staff will also check the wounds and make sure you are happy before you go home. Usually this will be about 2 hours after the surgery.
As a result of the local anaesthetic nerve block, your child may complain of a numb sensation in the groin and in some cases some weakness in the leg on the side of the surgery. This is temporary and will generally settle within a day or so of the operation.
Post-operative course
There may be a small amount of blood that oozes from the edges of the dressing, enough to lightly stain a nappy or pair of underpants. Paracetamol (‘Panadol’) should be given on the afternoon and evening of surgery, and in the morning of the following day. After that time, assess your child’s pain to see if further doses are required. Follow the manufacturer’s dose instruction but never give more than 4 doses in a 24-hour period and never both at the same time. Older children may require a stronger medication such as ‘Painstop Day-time’ if over one year of age. Your child should not be bathed on the first night, but nappies can be changed as required and a ‘wet-wipe’ or similar cloth used. Showers are safe from the next day onwards after the dresings have been covered by some cling film or Glad Wrap. There may be a small amount of blood that oozes from the wound under the dressing in the first 24 hours. Generally the dressing does not need to be changed, but if you are concerned please discuss with your local doctor or myself. It is quite normal for the scrotum and testis to swell after the operation and there may also be some bruising. This represents the body’s normal response to the operation and settles within the first few weeks.You should remove the dressing completely after a long bath on the fifth day after the operation. No further dressings are then required.
Your child can begin eating when he gets home. Start with clear liquids (apple juice, iceblocks) and add solid food slowly and in small amounts. Your child may vomit from the anaesthesia on the day of surgery. This should stop by the morning after surgery.
Return to activity
Your child may return to day care or school when comfortable, usually within 3-5 days. He should not participate in sports or swimming for 3 weeks after the surgery and should not ride straddle toys (bikes, walkers) for 2 full weeks after surgery. You should continue to use your car seat.
Call our office or contact the emergency department on given numbers if:
- You see any signs of infection: redness along the incision site, increased swelling, foul smelling discharge from incision
- Your child’s pain gets worse or is not relieved by painkillers
- There is bleeding (small ooze of blood in the first day or two is normal)
- Your child has a high temperature
- Vomiting continues on the day after surgery
- You have any questions or concerns
Follow up 4-6 weeks after surgery.
Follow-up
Normally I see you and your child about 4 to 6 weeks following surgery. This is both to ensure that the wounds have healed and that you and your son are satisfied with the results of the operation. Please ring soon after the operation to book the post operative appointment to arrange a convenient time. Boys are normally followed up for about 2 years after their surgery to make sure that the testis stays down as the boy grows.
Problems & further surgery
Generally this procedure is straightforward, but there is a 10% chance that the testis may not stay in the scrotum following surgery. In this situation a further operation will be required, usually about 6 to 12 months after the first procedure. During the operation there is a very small risk (less than 1%) of damage to the blood vessels to the testis and the sperm tube. This risk is minimised by the use of magnification during the procedure and usually can be both detected and repaired at the time of operation should this occur. As with any surgical procedure, there is always a 2-3% risk of a wound infection or bleeding after surgery. Any boy that has had an orchidopexy should wear a cricketbox when playing contact sports or sports which involve a hard ball. Also, after puberty, boys should be instructed to perform testicular self examination on a monthly basis because of the increased risk of testicular cancer in a previously undescended testes.


